Semaglutide represents a significant advancement in the pharmacological approach to weight management, functioning as a GLP-1 receptor agonist that mimics endogenous hormones to regulate appetite and insulin secretion.
Its mechanism of action not only supports weight loss but also addresses metabolic health, as evidenced by robust clinical data showing remarkable outcomes.
Understanding how semaglutide operates and its implications for long-term weight management is essential for those considering this treatment. Yet, the journey does not end with the science; various considerations must be explored to fully grasp its potential benefits and risks.
Semaglutide is a glucagon-like peptide-1 receptor agonist that has emerged as a pivotal medication in the management of obesity and weight loss. Initially developed for the treatment of diabetes, semaglutide has demonstrated efficacy in promoting weight reduction among individuals with obesity, regardless of diabetes status.
It mimics the action of the naturally occurring hormone GLP-1, which is involved in appetite regulation and glucose metabolism. Clinical studies have shown that patients using semaglutide experience substantial weight loss, improved metabolic health, and enhanced quality of life.
This medication is administered via subcutaneous injection, typically once weekly, making it a convenient option for long-term weight management. Its introduction has revolutionized obesity treatment protocols, offering a viable solution for many struggling with excess weight.
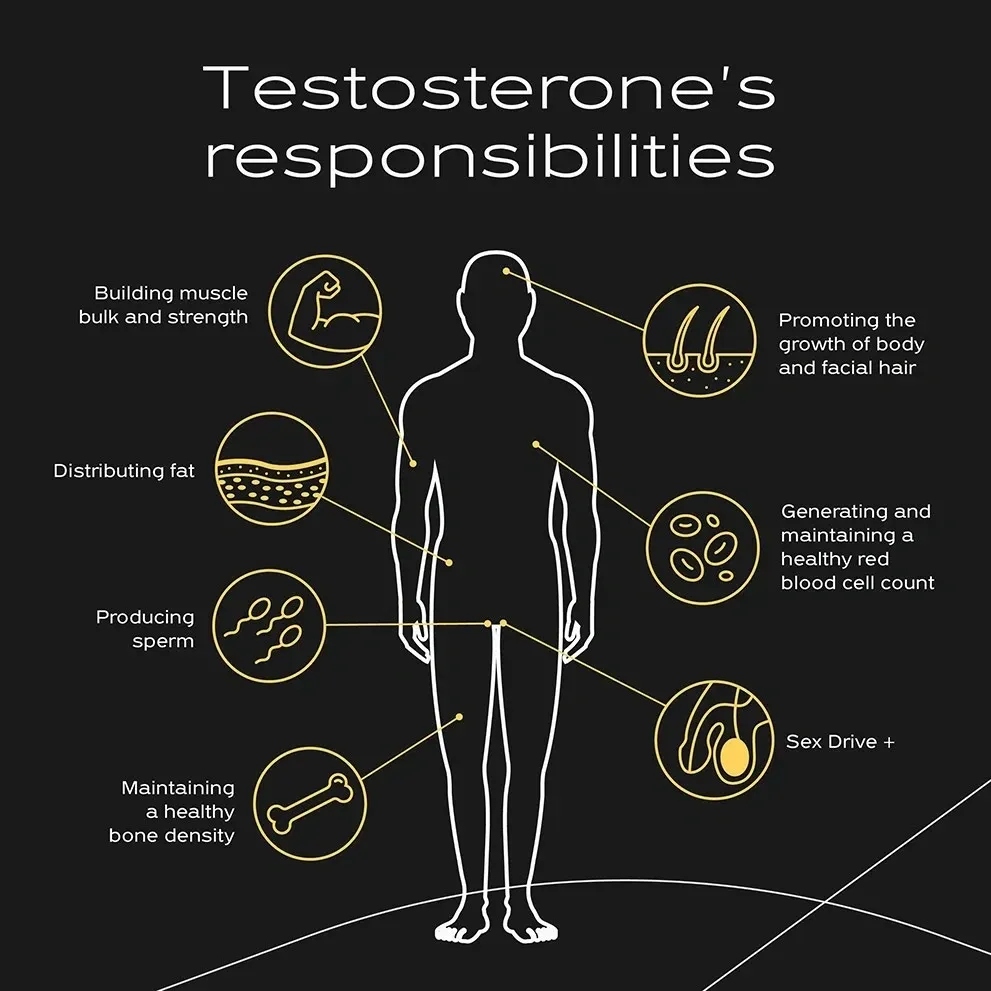
By mimicking the effects of the naturally occurring GLP-1 hormone, semaglutide enhances glucose-dependent insulin secretion and reduces glucagon release, thereby facilitating better blood sugar control. In addition, semaglutide slows gastric emptying, which promotes a feeling of fullness and decreases appetite.
This dual action not only helps in regulating blood glucose levels but also contributes to weight loss by reducing caloric intake. Moreover, semaglutide influences various brain regions involved in appetite regulation, enhancing satiety signals and diminishing hunger cues.
This extensive mechanism of action allows individuals to achieve significant weight loss while managing their glucose levels effectively. Overall, semaglutide represents an innovative approach to weight management and metabolic health, targeting multiple pathways for ideal results.

Clinical research has consistently demonstrated the efficacy of semaglutide in promoting weight loss among individuals with obesity or overweight conditions. In pivotal clinical trials, participants receiving semaglutide experienced significant weight reductions compared to those on a placebo.
For instance, the STEP trials revealed that adults administered semaglutide lost an average of 15% to 20% of their body weight over a 68-week period, showcasing the drug's potential as a long-term weight management solution.
Additionally, these studies indicated improvements in metabolic parameters, including reductions in waist circumference and enhanced glycemic control. The findings underscore semaglutide's role as a viable therapeutic option for individuals struggling to achieve sustainable weight loss, further emphasizing the need for ongoing research to optimize treatment strategies.
Releasing the potential for effective weight management is one of the primary benefits of semaglutide, which has emerged as a groundbreaking treatment for obesity. Clinical studies have demonstrated that semaglutide markedly aids in weight loss, with participants experiencing an average reduction of 15% to 20% of their body weight over a 68-week period.
This medication works by mimicking the action of GLP-1, a hormone that regulates appetite and food intake, thereby promoting feelings of fullness.
Additionally, semaglutide has been shown to improve metabolic health markers, such as blood sugar levels and cholesterol profiles. Its efficacy is further enhanced when combined with lifestyle modifications, making it an all-encompassing approach to achieving sustainable weight loss and overall health improvements.
While semaglutide offers significant benefits for weight loss, it is essential to take into account the potential side effects associated with its use. Common side effects include gastrointestinal issues such as nausea, vomiting, diarrhea, and constipation, which may diminish over time.
Some users may also experience abdominal pain or bloating. Additionally, there is a risk of more serious adverse effects, including pancreatitis and kidney impairment. Hypoglycemia can occur, particularly when used with other diabetes medications.
It is vital for individuals considering semaglutide to consult with healthcare professionals to discuss these potential risks and monitor their health throughout the treatment. Being aware of these side effects can help users make informed decisions regarding their weight loss journey.
Integrating semaglutide into a weight loss plan requires careful consideration and planning to maximize its effectiveness and guarantee safety. First, consult with a healthcare professional to determine if semaglutide is appropriate for your individual health profile.
Establish an all-encompassing weight loss strategy that includes a balanced diet and regular physical activity, as these lifestyle changes can enhance the medication's effects. Monitor your progress closely, adjusting dietary and exercise regimens as needed.
Regular follow-ups with your healthcare provider will allow for ongoing evaluation of your response to semaglutide, ensuring any potential side effects are managed promptly. Additionally, consider joining a support group or program to maintain motivation and accountability throughout your weight loss journey.
Genetics greatly influence an individual's propensity for weight gain, metabolism, and body composition. Genetic variations can affect appetite regulation, fat storage, and energy expenditure, thereby impacting weight loss efforts. While environment and lifestyle choices are essential, understanding genetic predispositions can provide insight into personalized weight loss strategies. Recognizing these genetic factors allows individuals to tailor their approaches, ensuring more effective and sustainable outcomes in their weight management endeavors.
Common weight loss myths include the belief that skipping meals accelerates weight loss, which often leads to overeating later. Another misconception is that all carbohydrates are detrimental; in reality, whole grains are beneficial. Additionally, some think that weight loss supplements are a quick fix, but they rarely replace the need for a balanced diet and exercise. Finally, the idea that fat-free foods automatically equate to healthier choices can lead to poor nutrition decisions.
Overcoming cravings for unhealthy foods requires a multifaceted approach. To begin with, identify triggers and develop a plan to manage them. Incorporate healthier alternatives, ensuring they are easily accessible. Staying hydrated and maintaining a balanced diet rich in nutrients can also diminish cravings. Mindfulness practices, such as meditation, can enhance self-awareness and emotional regulation. Finally, consider seeking support from professionals or support groups to cultivate long-term behavioral changes and accountability.